
According to the Skin Cancer Foundation, over 3.3 million people are diagnosed with and treated for skin cancer every year. Skin cancer can develop all over the body, especially in areas that receive the most sun exposure. As this progresses, it can become problematic for patients whose skin cancer is present on their face. However, when detected early enough, skin cancer can be treated and patients have a high cure rate. Mohs surgery is a specialized tissue-conserving reconstructive surgical method that progressively removes the affected tissues until only cancer-free skin tissue remains, which ensures complete cancer removal.
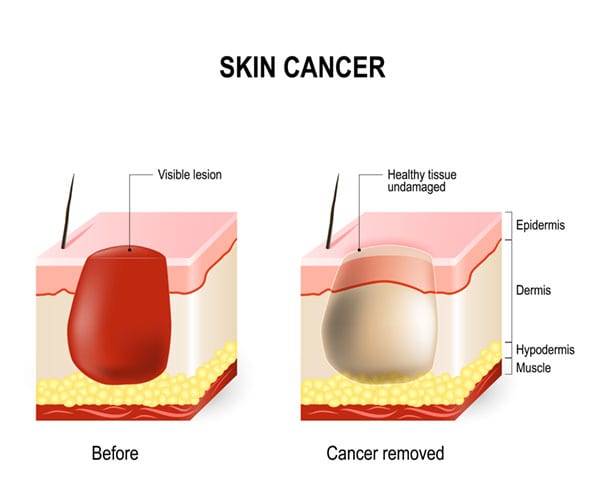
Certain skin cancer treatments can only estimate the amount of tissue to treat, which may result in the removal of healthy skin or tumor regrowth if any cancer is missed. Mohs surgery can successfully remove the affected areas and preserve as much healthy tissue as possible.
Mohs surgery is especially beneficial for patients with skin cancers in areas where tissue conservation, cosmetic, and functional outcomes are important. It is also indicated for recurrent cancers or cancers with potentially high recurrence rate.
This technique ensures that the least amount of tissue is removed while still enabling complete removal of the cancer. This allows for the smallest, least visible wound necessary for reconstruction.
Anticipated reconstructive options will be discussed with you at the time of your consultation. Options can include: direct closure, local flaps, or skin grafts. Very small superficial wounds can be allowed to heal by themselves.
Mohs surgery is performed on an outpatient basis using local anesthesia. A scalpel will be used to remove the visible tumor as well as a thin rim of tissue around the treatment site. The tissue will then be marked with dyes for orientation purposes while a map is made of the specimen. The tissue is prepared into an orange peel map so that the perimeter of the tumor can be evaluated. Once the prepared tissue has been analyzed by the surgeon, any remaining cancer that is identified will be marked and removed from the affected area. This procedure is repeated until the tumor is completely removed.
After the affected area has been removed, the tissues will be replaced to avoid leaving any large or unsightly holes in your face or body. Skin or cartilage grafts will be harvested from the head or other areas of the body. The grafted tissue is then carefully attached to the damaged areas and shaped and sculpted to blend in with your features. Stitches are used to close the wound, and a surgical dressing is placed over the treated area.
Following your Mohs surgery, you will experience some swelling and bruising depending on the treatment area, but this should resolve after a few weeks. Be sure you do not take any aspirin or nonsteroidal anti-inflammatory medication for at least three days. You will be asked to refrain from strenuous activity for up to three weeks. Be sure to avoid lying or sleeping on the side of the body treated with surgery. Follow-up appointments will be scheduled over several weeks following the procedure to ensure the wounds have healed properly.
Mohs surgery can provide patients with the best aesthetic results by removing the least amount of healthy tissue possible.
Scarring will depend on the amount of reconstruction needed and the treatment site. However, scars can be covered with makeup and are likely to fade over time.
You may experience discomfort as your wounds heal. You may take TYLENOL® or receive a prescription of TYLENOL® with codeine from your surgeon to help minimize the pain.
Get in contact with us below to schedule your MOHS surgery today.
Mohs surgery can be used to treat common skin cancers such as basal cell carcinoma and squamous cell carcinoma, as well as some more unusual skin cancers.
As with most surgical procedures, there are some risks associated with Mohs surgery. These can include:
Because Mohs surgery has a high success rate, most patients may only need one treatment.
Before and After Photos - individual results may vary
Some images may be models.
Site Designed & Hosted by Plastic Surgery Studios.
Vincent C. Hung, MD, FACS, INC. Copyright © 2024